Health insurance premiums under the Affordable Care Act (ACA) are set to rise in 2025, driven by a combination of inflation, increased drug costs, and consolidation within the healthcare market. Based on rate filings from 324 insurers across the U.S., the median proposed premium increase is around 7%, a figure that mirrors the increase observed in 2024. However, this broad statistic conceals significant variation across different states and insurers, with some rates rising by more than 10%, while others see decreases.
Distribution of Premium Changes
Looking closely at the data, premium changes range from significant decreases to moderate increases:
• Decrease of -10% to -15%: 3 insurers
• Decrease of -5% to -10%: 9 insurers
• Decrease of -5% to 0%: 38 insurers
• Increase of 0% to 5%: 76 insurers
• Increase of 5% to 10%: 113 insurers
As evident, the majority of insurers fall into the category of proposing increases between 5% to 10%, with 113 insurers proposing such changes. A substantial number, 76 insurers, are seeking smaller increases between 0% and 5%. Despite the relatively balanced spread, the wide variance—ranging from a 14% decrease to a 51% increase—reflects the different cost pressures that insurers face based on their regional markets and client demographics.
Key Drivers Behind Premium Increases in 2025
Several factors are contributing to the rising costs, including inflation, workforce shortages, market consolidation, and increased utilization of specialty drugs, particularly weight loss drugs. These factors are leading insurers to adjust premiums to cover anticipated higher healthcare costs.
1. Inflation and Medical Costs
Inflationary pressures are among the primary reasons for the rise in health insurance premiums. Healthcare costs, including the prices insurers pay for medical care and medications, have been rising steadily. As general economic inflation spiked between 2021 and 2023, the cost of healthcare services—often negotiated on longer-term contracts—lagged behind. By mid-2024, however, the increase in medical prices has caught up, outpacing general inflation. Many insurers, such as Independent Health Benefits Corporation in New York and Lifewise Health Plan in Washington, have cited inflation in their filings as a significant factor behind their rate increases.
2. Workforce Shortages and Market Consolidation
The healthcare industry continues to grapple with labor shortages, a problem exacerbated by the COVID-19 pandemic. Hospitals and other healthcare providers are facing higher labor costs and, in some cases, shortages of critical staff. This has led to hospitals and healthcare providers negotiating higher reimbursement rates from insurers. Hospital market consolidation is another contributor to premium hikes. As hospital systems merge and consolidate, they gain more negotiating power over insurers, demanding higher prices for their services. This effect is particularly pronounced in states like Oregon and New York, where insurers have highlighted the challenges posed by limited competition in their filings.
3. Weight Loss Drugs and Other Specialty Medications
The growing demand for GLP-1 drugs such as Ozempic and Wegovy, which are used to treat diabetes and promote weight loss, is another major driver of premium increases. While relatively few ACA insurers cover drugs approved exclusively for weight loss, such as Wegovy, the off-label use of diabetes drugs for weight loss is becoming more prevalent. Insurers like Blue Cross Blue Shield of Rhode Island and Priority Health in Michigan specifically noted the rising utilization of these drugs and their significant impact on pharmacy spending. In addition to weight loss medications, the increasing cost of specialty drugs and new gene therapies are also pushing premiums upward. Specialty drugs, which are often used to treat rare or complex conditions, account for a disproportionate share of total drug spending, despite being used by a relatively small percentage of the population.
Impacts of COVID-19 and Medicaid Unwinding
While the above factors are having a substantial impact on premiums for 2025, other potential drivers, such as COVID-19 and the unwinding of Medicaid continuous coverage, appear to be having little effect on premiums. As the nation moves further away from the height of the pandemic, insurers are reporting fewer costs related to COVID-19 treatment and testing. Most insurers noted that the impact of COVID-19 on their 2025 premiums is minimal.
Similarly, the end of Medicaid continuous enrollment, which began in April 2023, is having a muted effect on premiums. While millions of people have transitioned from Medicaid to ACA Marketplace coverage, most insurers reported that this shift has had little to no impact on their rate filings for 2025. However, a few insurers did report minor impacts, ranging from a 1-2% increase to a similar decrease in premiums as a result of the Medicaid unwinding process.
Geographic Variation and Insurer-Specific Differences
As in previous years, there is substantial variation in premium changes across different insurers and states. For example, while most insurers are proposing increases between 2% and 10%, a notable number are either reducing premiums or raising them more substantially. In the subset of insurers whose filings were reviewed in detail, those in states like Washington and Oregon were facing higher rate increases due to workforce shortages and hospital market consolidation, while insurers in other states, like New York, were seeing premium hikes due to rising drug costs.
The data on premium changes by insurer and state underscores the wide-ranging pressures facing the healthcare market. Some insurers are managing to keep their premium increases modest or even decrease rates, while others are forced to request substantial increases to cover rising costs.
The Role of Federal Subsidies and the Impact on Consumers
It is important to note that the vast majority of ACA Marketplace enrollees receive subsidies that help offset the cost of their premiums. As a result, many consumers will not directly experience the full impact of these rate increases. Federal subsidies are based on the benchmark silver plan in each state, and as premiums rise, so too does the amount the federal government spends on subsidies.
For most consumers, the out-of-pocket cost of their premiums will remain relatively stable, even as the overall cost of premiums continues to increase. However, higher premiums do mean higher federal spending, which has implications for the sustainability of the ACA program over the long term.
Distribution Of ACA Marketplace Premium Changes For 2025
Here is a bar chart visualizing the distribution of ACA Marketplace premium changes for 2025. The chart shows the number of insurers within each premium change category, ranging from decreases of -15% to increases of over 10%. This helps illustrate how the majority of insurers are proposing moderate increases, with fewer proposing significant decreases or substantial increases.
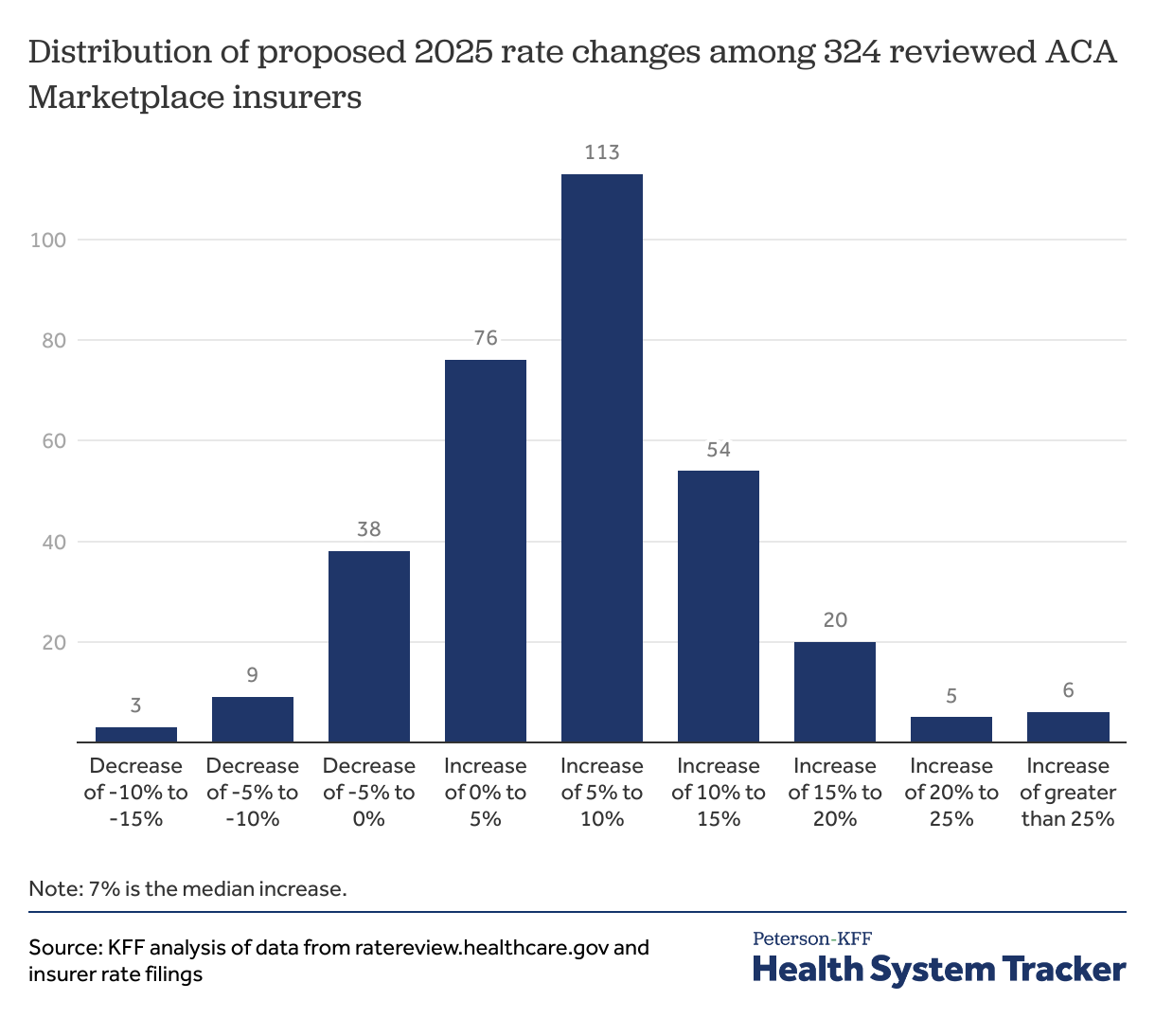
The ACA Marketplace premiums for 2025 are set to rise by a median of 7%, reflecting broader economic trends and specific pressures within the healthcare system. Inflation, rising medical costs, workforce shortages, hospital market consolidation, and the growing utilization of weight loss and specialty drugs are the primary drivers behind these increases. While some insurers are managing to keep premium hikes in check, others are facing double-digit increases due to these ongoing challenges.
Despite these increases, most consumers will be shielded from the full brunt of these changes due to federal subsidies. However, the continued rise in premiums raises questions about the future sustainability of the ACA Marketplace and the broader healthcare system's ability to contain costs in the face of growing economic and demographic pressures.

















 English (United States) ·
English (United States) ·