Sepsis is one of the most dangerous medical conditions that can affect anyone, yet it remains one of the least understood. Despite being responsible for more deaths annually than cancer, a new national survey by MedStar Health reveals that 81% of Americans are unaware of the symptoms of sepsis. This knowledge gap is a serious concern because recognizing sepsis symptoms quickly and seeking prompt medical attention can save lives.
In the United States alone, sepsis affects 1.7 million people each year, with at least 350,000 of those cases resulting in death. These alarming statistics underscore the importance of awareness, especially given that sepsis can rapidly escalate into a life-threatening condition in as little as 12 hours. To help bridge the knowledge gap, MedStar Health has developed the S.E.P.S.I.S. acronym, which provides an easy way for individuals to identify the symptoms of sepsis and take swift action.
What is Sepsis?
Sepsis is the body’s extreme response to an infection, which can be caused by bacteria, viruses, fungi, or parasites. When the body detects an infection, it triggers an immune response to fight off the invading organisms. However, in sepsis, this response becomes overwhelming and spreads throughout the body, leading to widespread inflammation. If left untreated, sepsis can result in tissue damage, organ failure, and death.
While sepsis can develop from any infection, common sources include respiratory infections like pneumonia, urinary tract infections (UTIs), skin infections from wounds or scrapes, and post-surgical infections. Even relatively minor infections can lead to sepsis if not addressed early, making it a sneaky and dangerous condition that can arise unexpectedly.
According to Dr. Jennifer Yu, sepsis physician lead for MedStar Health and critical care physician at MedStar Washington Hospital Center, "Sepsis takes a life every two minutes. It can look like a routine illness, then quickly change into a severe, life-threatening situation." This means that what may appear as a mild fever or discomfort could rapidly transform into a critical health emergency.
Why Awareness Matters
One of the most significant challenges in addressing sepsis is that it often goes unrecognized until it’s too late. Most cases of sepsis, about 80%, start outside of a hospital setting. This means that individuals may be suffering from sepsis at home without realizing the gravity of their condition. Each hour without treatment increases the risk of death by nearly 10%, highlighting the urgency of timely intervention.
Dr. Rollin J. (Terry) Fairbanks, senior vice president and chief quality & safety officer at MedStar Health, emphasized the need for early detection: "Sepsis is a sneaky disease. Almost any infection can lead to sepsis, and 80% of cases occur outside the hospital. Early recognition of symptoms that may be caused by sepsis can literally make the difference between life and death."
To help raise awareness, MedStar Health encourages people to remember the S.E.P.S.I.S. acronym, which highlights the key symptoms of sepsis that anyone can look for in themselves or others.
The S.E.P.S.I.S. Acronym
S — Shivering, fever, or very cold: Sepsis often begins with signs of infection, such as a fever or chills, but it can also present as an abnormally low body temperature (hypothermia), which is a sign that the body is struggling to regulate itself.
E — Extreme pain or discomfort: Unexplained or severe pain, often disproportionate to the original infection, can be an early indicator of sepsis.
P — Pale, discolored, clammy, or sweaty skin: Sepsis can interfere with the body’s circulation, leading to visible changes in the skin, such as paleness or a clammy texture.
S — Sleepy, confusion, or disorientation: Sepsis can impair brain function, leading to confusion, disorientation, or excessive sleepiness.
I — “I feel like I might die.”: A person with sepsis may have a strong sense that something is terribly wrong, often described as a feeling of impending doom.
S — Shortness of breath: Sepsis can affect the respiratory system, making it difficult to breathe and causing shortness of breath.
These symptoms may initially seem unrelated, but together they can signal the onset of sepsis. If you or someone you know experiences these signs, it’s crucial to seek medical attention immediately.
Who is at Risk?
Sepsis can affect anyone, but certain populations are at a higher risk. This includes infants and young children, older adults, individuals with chronic health conditions such as diabetes or chronic obstructive pulmonary disease (COPD), and those with weakened immune systems, including people undergoing chemotherapy or those with autoimmune disorders. Additionally, individuals recovering from surgery or those with open wounds are more susceptible to developing infections that can lead to sepsis.
Infections like pneumonia, UTIs, or even a dental infection can escalate into sepsis. Viral infections, such as COVID-19, have also been linked to sepsis, further complicating the battle against this deadly condition. The wide variety of potential causes means that everyone should be vigilant about monitoring symptoms, especially if they fall into one of the high-risk categories.
The Importance of Prompt Treatment
Early diagnosis and treatment are key to improving survival rates in sepsis cases. Once sepsis is suspected, medical professionals will typically conduct a thorough assessment that may include checking for physical signs like low blood pressure, increased heart rate, fever, and difficulty breathing. Blood tests can also be used to identify the presence of an infection and assess organ function.
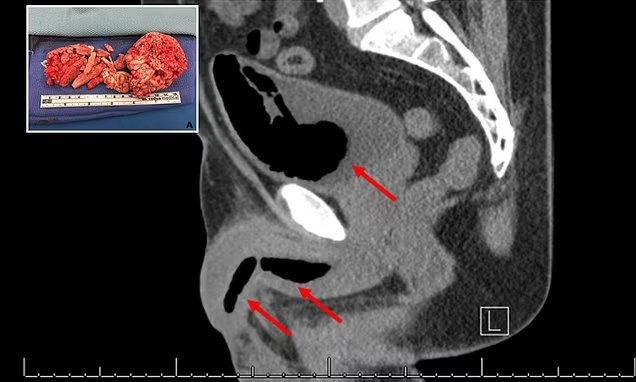
The most common treatment for sepsis is antibiotics, as bacterial infections are a leading cause. However, in some cases, antiviral or antifungal medications may be necessary. Oxygen therapy may also be required to support the body’s respiratory system, and in severe cases, surgery may be needed to remove the source of infection, such as an abscess or infected tissue.
In some cases, patients may require intravenous fluids to maintain blood pressure and ensure proper circulation. Advanced cases of sepsis may necessitate admission to an intensive care unit (ICU) for close monitoring and aggressive treatment. The complexity of sepsis treatment underscores why it’s so important to seek medical care as soon as possible.
How to Protect Yourself and Your Loved Ones
Since sepsis often develops from infections that start outside the hospital, it’s critical to be proactive about preventing infections in the first place. Proper wound care, good hygiene practices, and timely medical treatment for minor infections can go a long way in reducing the risk of sepsis.
For individuals at higher risk, extra precautions may be necessary. For example, those with chronic conditions like diabetes should work closely with their healthcare providers to manage their health and minimize the risk of infections. Similarly, individuals with weakened immune systems should take steps to avoid exposure to infectious agents, such as practicing social distancing during viral outbreaks or keeping up-to-date with vaccinations.
Another key strategy is to monitor the body for signs of infection and take immediate action if something seems off. Typical signs of infection include feeling unwell, fever or a sudden change in body temperature, and pain, redness, discharge, or swelling near a wound or surgical site. Flu-like symptoms, such as a sore throat, vomiting, or diarrhea, should also be taken seriously, as they may indicate an infection that could lead to sepsis.
Sepsis in the Era of COVID-19
The COVID-19 pandemic has highlighted the dangers of viral infections leading to severe complications, including sepsis. While much of the focus has been on respiratory symptoms and lung damage, COVID-19 can also trigger an overwhelming immune response that results in sepsis. This is particularly true for individuals with preexisting health conditions or those in older age groups.
In light of this, it’s essential to understand that sepsis is not solely caused by bacterial infections. Viruses, including COVID-19, can also set off the chain reaction that leads to sepsis, making it all the more important to be vigilant about symptoms and seek medical care when necessary.
Conclusion
Sepsis is a silent killer that claims hundreds of thousands of lives each year, yet it remains underrecognized and misunderstood by the majority of Americans. The good news is that awareness can make a difference. By remembering the S.E.P.S.I.S. acronym, individuals can better identify the early warning signs of sepsis and seek life-saving treatment.
Whether caused by a bacterial infection, a virus like COVID-19, or even a minor cut or scrape, sepsis can develop rapidly and requires immediate medical intervention. With prompt treatment, including antibiotics and supportive care, the chances of survival significantly improve.
As we observe Sepsis Awareness Month, it’s crucial to spread the word about this life-threatening condition. By increasing public awareness and encouraging people to seek timely medical attention, we can reduce the toll that sepsis takes on our communities. The key to survival lies in recognizing the symptoms and acting fast—because when it comes to sepsis, every second counts.
















 English (United States) ·
English (United States) ·