VERIFY is answering some of the most common questions about how monkeypox spreads, vaccine availability, and whether any deaths have been reported.
A man in Massachusetts tested positive for monkeypox on May 18, becoming the first U.S. case in 2022. Since then, thousands of monkeypox cases have been reported throughout the country.
Nearly 80 other countries have also reported tens of thousands of monkeypox cases as of Aug. 1, 2022.
The global monkeypox outbreak has prompted many questions from VERIFY readers, including how the virus spreads, whether vaccines are available, and if any deaths have been reported.
We are answering some of the most common questions about the monkeypox outbreak.
THE SOURCES
FAST FACTS
WHAT WE FOUND
How does monkeypox spread?
The CDC says monkeypox is transmitted when a person comes into contact with the virus from an animal, human, or materials that are contaminated with the virus.
The virus enters the body through broken skin (even if not visible), the respiratory tract, or the mucous membranes (eyes, nose, or mouth).
Animal-to-human contact can occur if an infected animal bites or scratches a person. Human-to-human transmission primarily occurs through close physical contact with bodily fluids, respiratory droplets, skin lesions or recently contaminated objects, the CDC and World Health Organization (WHO) say.
Monkeypox often spreads through skin-to-skin contact and many, though not all, cases have been among men who have sex with men. The virus can also spread from coming in contact with clothing, bedding or other items used by an infected person, though this is much less common.
“The act of putting clothes on and removing them can scrape the skin. So, if someone with active monkeypox lesions tries on clothes and then someone else tries them afterward, there is a chance they can contract monkeypox,” Ilhem Messaoudi Powers, an immunologist at the University of Kentucky College of Medicine, told VERIFY. “This is because some of the lesions can release their fluid, which is often full of live virus particles. This is the same for hotel room sheets and towels.”
Messaoudi explained that it is currently difficult to determine how long the virus stays on clothes and linen after they have come in contact with an infected person, but she said contaminated clothing and bedding “should be cleaned thoroughly to avoid transmission.”
Is monkeypox considered a sexually transmitted disease?
Though monkeypox can be transmitted through sexual contact, it is not considered a sexually transmitted disease and is not on the WHO’s list of viruses transmitted through sexual contact.
There are no sexually transmitted diseases known to have originated within the orthopoxvirus family, of which monkeypox is a member, according to a list from the National Institute of Health.
Other viruses that can spread during sex, but are not considered sexually transmitted disease (or STDs), are:
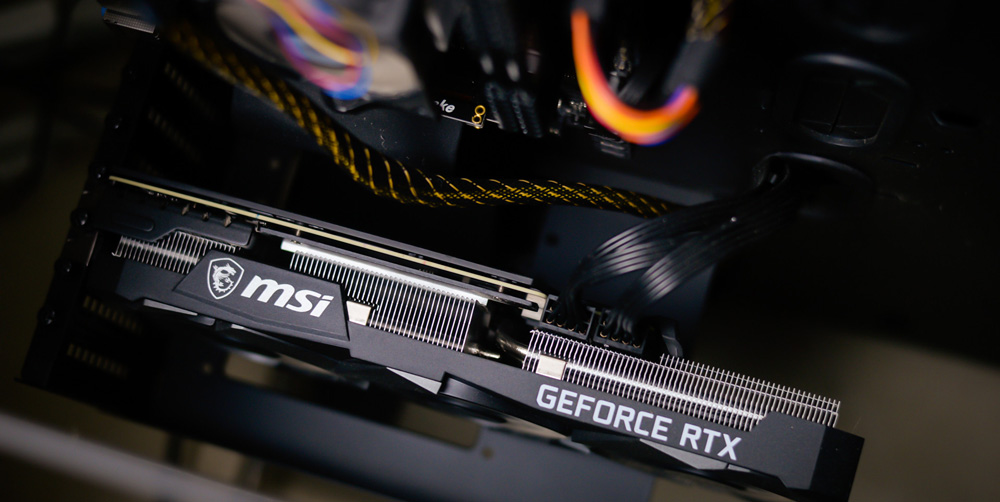
What are the symptoms of monkeypox?
Most patients with monkeypox experience fever, rash and swollen lymph nodes, according to the WHO. The rash tends to stay concentrated on the face and limbs, but can spread across the body in more severe cases.
Other symptoms of monkeypox include headache, chills, fatigue, and respiratory symptoms such as sore throat, nasal congestion and cough, the CDC says.
Has anyone died from monkeypox during the 2022 outbreak?
As of July 22, 2022, five deaths from monkeypox in the African region had been reported to the WHO.
On July 30, Spain reported its second death from monkeypox shortly after the first, which are believed to be the first confirmed fatalities from the disease in Europe, according to the Associated Press. Brazil has also reported at least one death from monkeypox, the AP said.
There have been zero confirmed monkeypox deaths so far in the U.S., according to the CDC and WHO.
According to the WHO, the monkeypox death rate has historically ranged from 0 to 11% in the general population and has been higher among young children. In recent times, the death rate has been around 3-6%.
The death rate for the current outbreak has not yet been established.
How long should people with monkeypox isolate themselves?
The CDC recommends that people with monkeypox remain isolated at home or another location for the duration of the illness, since current data suggest people can spread the virus from the time symptoms begin until they have resolved.
According to the WHO and CDC, symptoms typically last two to four weeks. A person’s symptoms have resolved once they don’t have a fever or other respiratory issues, and the rash has fully healed with a fresh layer of skin formed over it.
The CDC has guidance on its website for those who are unable to remain fully isolated throughout their illness.
Are there vaccines for monkeypox?
Since monkeypox is “closely related” to the virus that causes smallpox, smallpox vaccines “can protect people from getting monkeypox,” according to the CDC.
Data from past studies show that the smallpox vaccine is about 85% effective in preventing monkeypox when given before someone is exposed to the virus, the WHO and CDC say. The vaccine can also be effective at preventing illness or reducing symptom severity if it is given shortly after someone is exposed to monkeypox.
The U.S. Food and Drug Administration (FDA) has licensed two vaccines to prevent smallpox: ACAM2000 and Jynneos.
The ACAM2000 vaccine is approved by the FDA for use in smallpox prevention, but the CDC has expanded access to allow its use for monkeypox as well, according to the U.S. Department of Health and Human Services.
The Jynneos vaccine was approved by the FDA in September 2019 for use in the prevention of both smallpox and monkeypox disease.
People with inflammatory skin conditions such as eczema, as well as those with weakened immune systems, should only use the Jynneos vaccine, the CDC says.
Vaccines are limited right now to those who are most at risk of being infected with monkeypox, including people who were exposed to someone who has monkeypox, people who have had multiple or anonymous sexual partners, and men who have sex with men.
Local and state health departments are determining vaccine eligibility during the current outbreak, so requirements may vary based on where a person lives. People who have questions about their eligibility should contact their local health department.
If I was previously vaccinated against smallpox, will it protect against monkeypox?
Routine smallpox vaccinations used to be commonplace in the United States, but this practice stopped in 1972 after the disease was eradicated in the country, the CDC says. That means smallpox vaccines aren’t available to the general public anymore. Those who have previously been vaccinated against smallpox can usually find evidence as a scar on their upper arm, according to the WHO.
So what does a previous smallpox vaccination mean during the current monkeypox outbreak?
Though previous vaccination provides protection against monkeypox, it may not be lifelong, according to the CDC. During the 2003 monkeypox outbreak and the current outbreak, some people who had received the smallpox vaccine decades ago were infected with monkeypox.
Stuart Ray, M.D., a professor at Johns Hopkins Medicine, agrees.
“What we don't know is whether or at what point people who have had decades since that [smallpox] vaccination, or have become immunosuppressed since that vaccination, might become susceptible,” he said.
Has the monkeypox outbreak been declared a pandemic?
The WHO is responsible for declaring a pandemic. Right now, the public health agency is referring to the monkeypox situation as a “multi-country monkeypox outbreak,” not a pandemic, a spokesperson told VERIFY.
The CDC and White House also refer to monkeypox as an “outbreak.”
Though the monkeypox outbreak is not considered a pandemic, the WHO has declared it a Public Health Emergency of International Concern (PHEIC). This is the highest level of alert that the public health agency can issue.
A PHEIC is defined as “an extraordinary event which is a public health risk to countries through cross-border spread, and which requires a coordinated international response," according to a spokesperson for the WHO.
COVID-19 reached the level of a PHEIC about two months before it was declared a pandemic.
If monkeypox is eventually declared a pandemic, it won’t be “anything like the scale that we’re seeing for COVID” due to several factors, including how the viruses spread, Kathryn Jacobsen, an infectious disease epidemiologist and professor of health studies at the University of Richmond, said.
“Coronavirus spreads through the air, so it's really easy for that to spread into crowds because it goes through the air system. …In very close proximity, it is possible for [monkeypox] to spread without touch,” she said. “But it does not appear to be something that aerosolizes or spreads widely through the air. It's mostly skin-to-skin contact, which means that it isn't going to spread nearly as fast as coronavirus spread.”
Can the COVID-19 vaccine give someone monkeypox?
Because monkeypox is currently uncommon, some online users have questioned how it’s transmitted and if there could be a connection to other viruses, like the ones that cause shingles and COVID-19. Others have asked if the COVID-19 vaccine could have actually caused the monkeypox outbreak.
Chickenpox and shingles are members of the herpes virus family, and monkeypox and smallpox are orthopoxviruses. The vaccine that protects against COVID-19 does not contain any live viruses and has no connection whatsoever to herpes viruses or orthopoxviruses, Messaoudi told VERIFY.
There are rare cases when the COVID-19 vaccine could trigger a shingles flare-up in people who were previously infected with chickenpox. Shingles causes a painful, burning rash, along with other symptoms, due to the reactivation of the chickenpox virus.














 English (United States) ·
English (United States) ·